It’s one of the most common questions men ask when they’re told they have an enlarged prostate:
“Can BPH turn into prostate cancer?”
The short answer is no — but understanding the difference between the two conditions can ease a lot of worry and help you make informed decisions about your health.
BPH and Prostate Cancer: Different Conditions, Same Organ
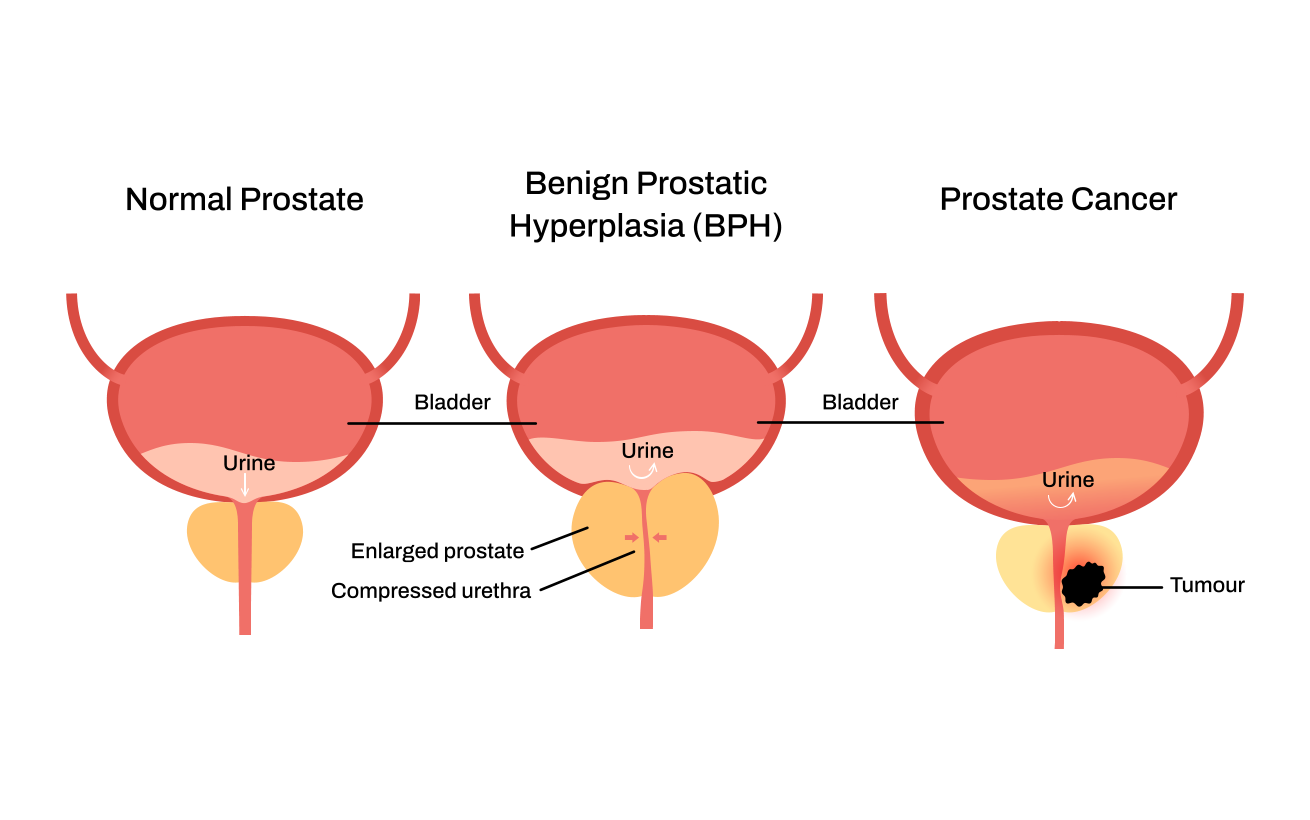
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland. It’s caused by normal hormonal changes that come with age and affects the part of the prostate surrounding the urethra — the channel that carries urine out of the body. As the gland grows, it can press on the urethra and cause symptoms such as:
- A weak or interrupted urine stream
- Frequent or urgent need to urinate
- Getting up several times at night to urinate (nocturia)
- Difficulty starting urination
Prostate cancer, on the other hand, is made up of regular prostate cells that, for reasons that are unclear, begin to grow and divide uncontrollably. These cells look different from healthy ones and form a tumour.
Usually, prostate cancer starts at the outer edge of the prostate and grows inward, whereas BPH begins in the central area around the urinary passage and grows outward. Depending on the size and location of the cancer, there may be no symptoms at all (sometimes it’s detected only because of a high PSA) – or symptoms can mimic those of BPH.
If not detected early, prostate cancer can spread locally, just outside the prostate, or further away to the lymph nodes, bones, liver, or other areas (a process called metastasis).
Can One Lead to the Other?
Although BPH and prostate cancer can occur at the same time, one does not cause the other. Having BPH does not increase your risk of developing prostate cancer. However, because both conditions affect the same organ and may cause overlapping urinary symptoms, it’s important to distinguish between them through proper testing.
Why Testing Matters
Even though BPH is benign, similar symptoms – such as frequent urination or difficulty emptying the bladder – can also appear with prostate cancer. That’s why screening is essential.
Your urologist may recommend:
- A PSA (Prostate-Specific Antigen) blood test
- A digital rectal exam (DRE)
- Imaging or, in some cases, a prostate biopsy
These tools help identify whether your symptoms are caused by BPH, prostate cancer, or — in some cases — both conditions occurring together.
Note: having BPH does not cause cancer; but because both are common in aging men, they can sometimes be present simultaneously.
Managing BPH
If your tests confirm BPH, several minimally invasive treatments are available — including Rezūm, iTind, and Optilume. Each works differently to relieve urinary symptoms and improve quality of life without major surgery. The choice of treatment depends on several factors, which your urologist will discuss with you in detail to ensure the best fit for your needs and goals.
The Bottom Line
BPH and prostate cancer are two separate conditions. BPH does not turn into cancer, but the symptoms can be similar — so evaluation by a urologist is the only way to know for sure.
If you have questions about your test results, our specialists at University Urology Associates will review your findings, explain your options, and guide you toward relief with clarity and confidence.
Book a consultation or complete our 4-question BPH quiz to find out whether you may benefit from our minimally invasive treatments.